Excerpt from Cyndi O’Meara’s article on Wellness Daily website
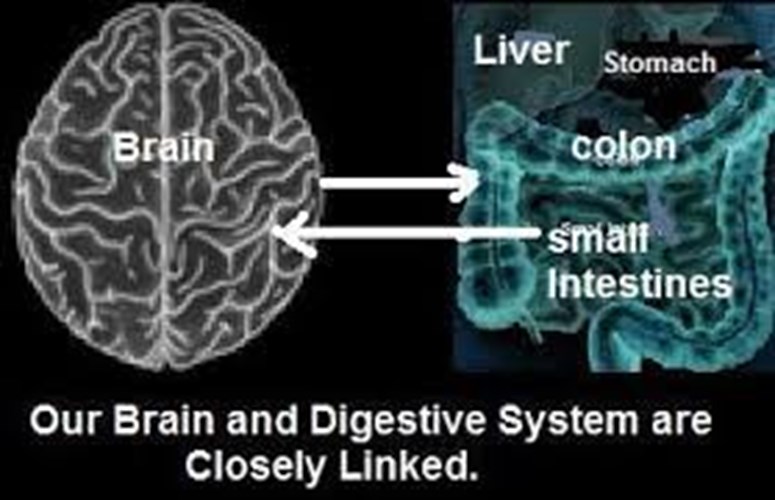
Scientific knowledge and understanding is expanding at an exciting pace. The connection between what we eat and its effect on what we think is no longer in question, yet there is so much more to learn, understand and implement from this emerging field of Gut- Brain connection.
You most likely have experienced nervous butterflies at the start of a race or just thinking about speaking in front of a large audience. You have probably also eaten and drunk too much and had brain fog the next day. These everyday examples of the gut-brain connection working in both directions can be familiar to us.
Cyndi O’Meara explains that, Stress, inflammation, a sluggish vagus nerve in your enteric nervous system and the microbiome in the gut all play a role in this phenomenon. Messengers continually go between the gut and the brain.
What stands out the most is the integrity and diversity of the microbiome, that group of organisms that live in your gut. They weigh more than the human brain and can make nutrients (vitamins B, K and fats), enhance the immune system, digest our food and produce the precursors for the brain and nervous system's messengers.
Ninety percent of serotonin and 50 percent of dopamine are found in the gut. An imbalance of these neurotransmitters is implicated in anxiety and depression. Yet when a patient presents to a psychiatrist there is very seldom talk of the gut, bowel movements and digestion. A holistic approach would prove more beneficial.
The microbiome is now being implicated in anxiety, depression, learning and memory, appetite and satiety, and much more.
By keeping our microbiome healthy and happy, we in turn keep our brain, thoughts and feelings more in check.
Depression, anxiety and other mental disorders described in the Diagnostic and Statistical Manual of Mental Disorders have been increasing. On average in Australia one in four adults have been prescribed an antidepressant in 2017. These medications are reaching a younger audience, with children under the age of 10 being diagnosed with depression and anxiety and prescribed medications.
The science behind the connection between the brain and the gut will hopefully turn psychiatry practice around. Instead of looking at the brain alone there needs to be more focus on the gut. The increase in mental disorders aligns with the decrease in gut health and diversity of the microbiome. Antibiotics in food and taken by prescription, glyphosate (herbicide/antibiotic sprayed on grains, legumes and seeds), refined packaged food like substances that are eaten by the masses and a lack of prebiotics and probiotics via the food chain have been a disaster to the microbiome and it’s diversity; couple that with an increase in C-sections and a decrease in breastfeeding, these all change the babies microbiome for life.
A rise in mental health is not surprising when we consider the significant changes away from a whole food, plant-based diet that was normal 50 to 100 years ago. Highly refined processed foods laden with sugar, salt, hydrogenated fat, flavours and preservatives along with traces of herbicides, pesticides and plastics are having an impact. Antibiotics and other medication also disrupt the healthy gut flora.
It is becoming increasingly clear that the initial seeding of the microbiome at birth is crucial for long-term physical and mental health. Not only are our brains affected by the dysbiosis of the microbiome, but there is an increase in gut disorders, including; inflammatory bowel disease, fructose malabsorption, Small intestinal bacterial overgrowth (SIBO), ulcerative colitis, celiac disease and more. There is also an association with skin conditions, allergies, food sensitivities, asthma and autoimmune disorders.
Awareness is the first step, the next step is doing something about it. O’Meara suggests these steps.
Add movement, sunshine, connection and clean water to this formula and you might find a ray of sunshine bursts through that hazy, tired anxious brain.
Cyndi O’Meara is a nutritionist, best-selling author, real food advocate, international speaker, filmmaker (What’s With Wheat).